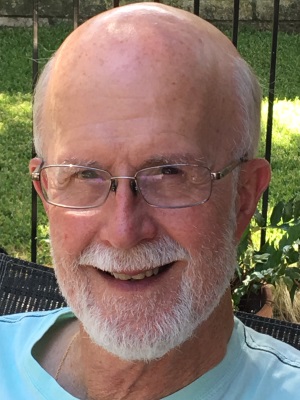
I received my PhD from the University of North Texas in 1976 and was licensed as a psychologist in 1978. My first six years of practice was spent in community mental health centers around the state of Texas. At one point, I was the Chief Psychologist at Wichita Falls Stated Hospital for four years. These early experiences prepared me to function in a variety of clinical settings with a widely diverse population of patients.
In 1989, I entered the private sector, as a staff psychologist at the Center for Psychiatric Medicine in Houston, Texas, treating patients with chronic pain both as inpatients and outpatients. Patients were taught self-management skills and educated about pain and maximizing the quality of life with pain. I also ran a group for family members with a focus on adjusting to the impact of chronic pain on the family. My experience there strengthened my awareness of the connection between mind and body and the importance of addressing both in treatment.
In 1992, I joined the staff at St David’s Rehabilitation Hospital in Austin, Texas as a psychologist in the inpatient pain management program. That program was similar to the one at CPM. Three years later, the program was discontinued and I was absorbed into the inpatient rehabilitation program. For the next eighteen years, I worked with literally hundreds of patients and their families who suddenly found themselves facing adjustment to life changing, often catastrophic, injuries and illnesses. Most of the patients there were experiencing severe trauma and pain as well. Many patients and families were delighted to be treated by a Christian psychologist at a time of crisis in which their faith was seen as a resource and incorporated into the adjustment and healing process.
Since 2013, I have maintained a private outpatient psychology practice with a focus on treating individuals with trauma, PTSD, persistent pain, and chronic, often debilitating illness.
My interest in chronic pain is personal. I experienced persistent low back pain for thirty-five years as a result of two motorcycle incidents. I know firsthand how limiting pain can be and how important it is to do regular self-maintenance such as exercise, pacing, stretching and practicing good body mechanics, good nutrition and stress management. I practice what I preach. I have exercised most days since September of 1976. I love hiking and photography. Rocky Mountain National Park is one of my favorite places in the world. The trails in Georgetown, Texas are pretty great, too.
As I work with people, I view them through the lens of adaptation, i.e., always doing the best they can, given their life experiences rather than seeing them as being sick, dysfunctional or some other way that engenders guilt, shame, or blame. I carry hope, encouragement, humor and joy and share those with my patients. My goal for each person I treat is to release them to be able to choose to be the best version of themselves that they can be.
I maintain my vision of hope and joy through my faith in God, my loving wife and family, exercise and my childlike fascination with nature – where I spend as much time as I possible can.